 Intelligent Design
Intelligent Design
 Medicine
Medicine
Cardiovascular Function: The Heart Follows the Rules
Editor’s note: Physicians have a special place among the thinkers who have elaborated the argument for intelligent design. Perhaps that’s because, more than evolutionary biologists, they are familiar with the challenges of maintaining a functioning complex system, the human body. With that in mind, Evolution News & Views is delighted to present this series, “The Designed Body.” For the complete series, see here. Dr. Glicksman practices palliative medicine for a hospice organization.
 The body is made up of atoms and molecules that must follow the laws of nature. These laws demand that each of the body’s trillions of cells must have enough energy and different chemicals to live, grow, and work properly. To this end, the body has a cardiovascular system that sends blood to the cells to give them what they need.
The body is made up of atoms and molecules that must follow the laws of nature. These laws demand that each of the body’s trillions of cells must have enough energy and different chemicals to live, grow, and work properly. To this end, the body has a cardiovascular system that sends blood to the cells to give them what they need.
So far in this series we’ve seen that in order to have enough blood volume, there must be enough water and sodium in the right places. Maintaining the proper resting membrane potential for heart, nerve, and muscle function requires control of the body’s potassium as well. Now we need to look at how the body moves the blood to where it needs to go. After all, blood has mass and, like all matter, requires energy to be moved against the natural forces of inertia, friction, and gravity. To follow the rules the body uses the heart to pump blood throughout the cardiovascular system. Let’s see how that works.
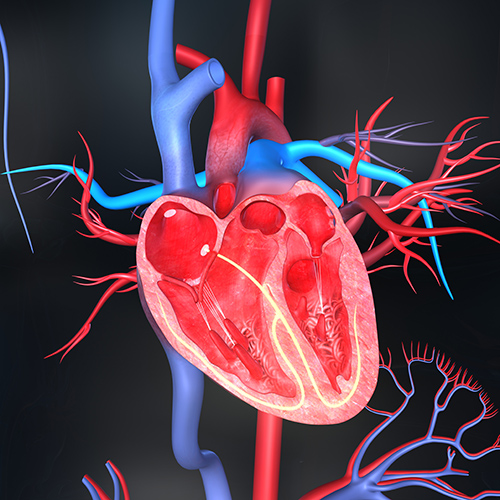
The heart is a muscular pump that is divided into a right and left side by a wall called the septum. Each side of the heart consists of a thin-walled upper chamber, called the atrium, and a more muscular lower chamber, called the ventricle. There are “V”-shaped one-way valves that point in the direction of blood flow between the atria and the ventricles, and the ventricles and their outflow tracts. When the valves open, they direct blood forward to where it is supposed to go. When they close, they prevent blood from going backward to where it is not supposed to go.
The right ventricle pumps blood through the main pulmonary artery to the lungs while the left ventricle pumps through the aorta to the rest of the body. Because it has to pump the blood farther, the left ventricle needs more muscle thickness and power than the the right ventricle. Muscles usually need to be stimulated by nerves to contract. However, even though the nervous system can modify its function, the heart is a unique muscle that is able to march to its own drummer.
Recall that, due to more K+ ions leaking out of the cell than Na+ ions leaking in, the inside of the plasma membrane carries a negative electrical charge while the outside carries a positive one. This difference in the electrical charge across the plasma membrane is called the resting membrane potential. Nerve and muscle cells are considered excitable because, when adequately stimulated, they can depolarize which means they reverse the polarity of their membrane potential. Thus the inside of the plasma membrane becomes positive and the outside becomes negative. This happens because the stimulus triggers Na+ ions to quickly flood into the cell.
Depolarization signals the nerve cell to release its neurohormone and the muscle cell to contract. After depolarization takes place the nerve and muscle cells repolarize by stopping Na+ ions from entering and letting K+ ions leave the cell. This returns the membrane potential to normal. But at the end of this process the net Na+ ion concentration in the cell rises and the net K+ ion concentration falls.
If this were not reversed, after several depolarization-repolarization events, the chemical content of the cell would drastically change, leading to neuromuscular malfunction. In fact, it is the sodium-potassium pumps in the plasma membrane that correct the Na+ and K+ ion concentrations by pushing three Na+ ions out for every two K+ ions brought back in. So the sodium-potassium pump not only controls the cell volume and maintains the 2/3:1/3 ratio between the fluid inside and outside the cells, but by maintaining the Na+ and K+ ion concentration, it also preserves nerve and muscle function.
In general, skeletal muscle cells, under voluntary control, depolarize and contract after being adequately stimulated by neurohormones released from nerve cells. But many of the cells in the heart can depolarize automatically. This takes place because, without having to be stimulated, these heart cells allow Na+ ions to leak into the cell at a faster rate than regular muscle cells. The speed at which this Na+ ion leakage into the cell takes place determines how fast the cell will depolarize and cause muscle contraction.
The sino-atrial node, high up within the right atrium, acts as a natural pacemaker and normally dominates and controls the heart rate because its cells leak Na+ ions in faster than any of the other cells of the heart. Once these pacemaker cells depolarize, they send an electrical signal through the conducting system to the other heart cells and depolarize them, which causes them to contract and pump the blood where it needs to go. It is important to note here that heart muscle contraction is different from skeletal muscle contraction in that its rate of depolarization and strength of contraction are related to not only the entry of Na+ ions into the cell, but calcium ions (Ca ++) as well.
The cardiac cycle consists of systole (contraction), which takes up about one-third of the time, and diastole (relaxation), which takes up the remaining two-thirds. When the sino-atrial node fires, its electrical message passes through the atria and the conducting system to the ventricles and they start to contract. This begins the systolic phase of the cardiac cycle.
Early on, the valves between the atria and the ventricles close, preventing blood from going back into the atria. Soon after, the valves to the outflow tracts open and blood is pumped from the right side of the heart, through the main pulmonary artery to the lungs, and from the left side of the heart, through the aorta to the rest of the body. At the end of the systolic phase, the valves between the ventricles and their outflow tracts snap shut to keep the blood in the main pulmonary artery and the aorta from going back into the ventricles. After the ventricles finish contracting, they begin to relax, which starts the diastolic phase of the cardiac cycle.
Early in diastole, the valves between the atria and the ventricles open to allow the blood returning to the heart from the veins to also flow into the ventricles. The atria and ventricles slowly fill up with blood during this relaxation phase and near its end, the sino-atrial node fires. This electrical message stimulates the atria to contract, pushing more blood into the ventricles. The signal then moves from the atria through the conducting system to stimulate the ventricles to contract and the cardiac cycle begins again.
Now that you understand how the heart works, it is important to consider what it must be able to do to keep us alive. After all, experience teaches that when we are very active, doing things like running, jumping, climbing, lifting, or hauling, our heart automatically beats faster and harder to give our muscles the energy they need. The hearts of our earliest ancestors would need to have been able to do the same thing for them so that they could win the battle for survival. This means that, when it comes to heart function and living within the laws of nature, the body must take control so it can do what it needs to do to survive. We’ll see how the body does that next time.
Image: � 7activestudio / Dollar Photo Club.
